Pancreas: The Sugar Regulator
THE PANCREAS (REVISITED)
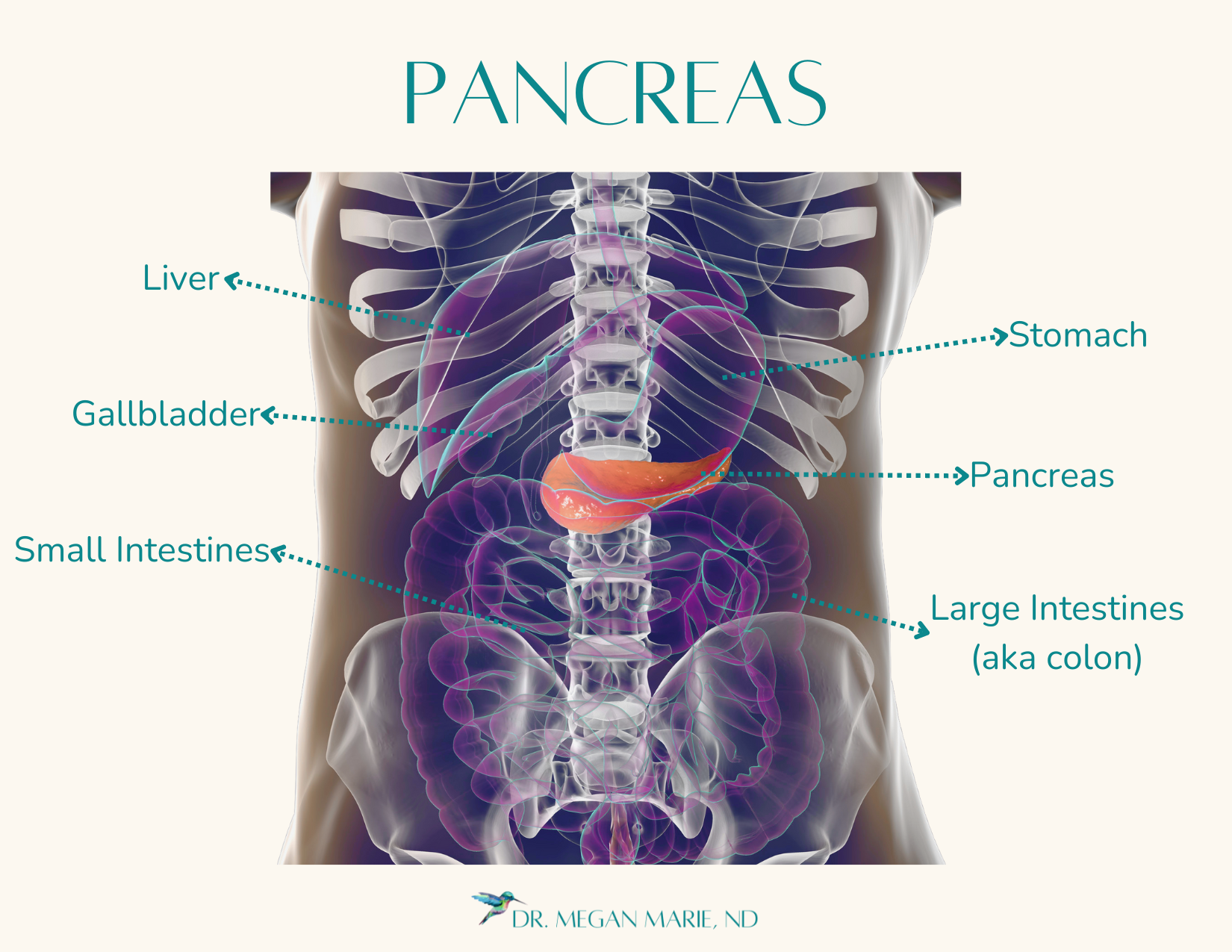
Welcome back to our “Tour of the Body” series! As we learned in the digestive system tour, the pancreas has two roles: making digestive enzymes and releasing blood sugar managing hormones, revisit that post here. As a reminder, the head of your pancreas is located 3-6in straight up from your belly button, and spans to the left behind your stomach.
BLOOD SUGAR REGULATION 101
Why does sugar in our blood matter anyway? Glucose (sugar) is the primary source of energy for nearly all the cells in your body. Especially our brain, which can’t store energy like our muscles can. This is often why we get the munchies when we’re studying, our brain has literally burned up sugar processing new information. If blood sugar drops too low (hypoglycemia) it can cause confusion, dizziness, and even fainting because the brain doesn’t have enough “fuel” to operate.
We keep our blood sugar regulated via the hormonal actions of insulin, glucagon, and somatostatin.
GLUCAGON
If our blood sugar is low (because we’re fasting or just exercised), the pancreas releases glucagon. Glucagon signals to the liver “hey, release your glycogen stores, we need more sugar out here!” Glycogen (stored sugar) is a stop-gap. Glycogen stores can typically last 12 to 24 hours in a resting state (or about 1-3 hours depending on exercise intensity), it’s not a meal replacement mechanism. Think about it more like your gas gage being on empty…you can “run on fumes” for only so long before the car stops. (FYI: you also have muscle glycogen, but that’s reserved for muscle use only and doesn’t contribute directly to blood sugar levels.)
SOMATOSTATIN
Is a regulatory hormone that acts as an inhibitory or “braking” signal in the body. It’s produced in many areas of the body, including the hypothalamus, digestive tract, and of course, the pancreas. This is especially important in digestion, as it regulates how fast our food is broken down and absorbed. It also helps balance how much thyroid stimulating hormone is released (keeping our metabolism in balance), as well as many other hormones.
In response to high blood sugar, somatostatin is released to inhibit further increase, helping to maintain blood sugar balance.
INSULIN
When we eat, our blood sugar goes up, and the pancreas responds by releasing insulin. Insulin acts like a key, unlocking cells so they can absorb glucose from the bloodstream, to be used as energy by our muscles, tissues, and brain. This is the healthy response: we eat, blood sugar levels go up, insulin is released, blood sugar comes back down, and the energy from food is used to live life.
However, because our connection to food and moderation has shifted in the modern world, insulin can easily become imbalanced. Factors like overeating, consuming too many sugary foods or beverages, eating processed foods, or junk “foods”—non-food confabulations that the body doesn’t recognize—can overwhelm the system. When this happens, the body ends up producing more insulin to deal with the excess of sugar in the blood. Over time, this overproduction leads to insulin resistance.
INSULIN RESISTANCE
This is when cells stop responding to insulin’s signal; the key just doesn’t open the lock. As a result, sugar remains in the bloodstream because the cells aren’t taking it in (they have enough). But the body doesn’t want the sugar in the bloodstream either. This causes the pancreas to release even more insulin in another attempt to get the sugar out of the blood. This leads to chronically high insulin levels and eventually high blood sugar, as the body struggles to manage the excess. The body’s cells are resistant to insulin.
High blood sugar is more than just an energy imbalance—it triggers inflammation throughout the body. When sugar levels are too high, they can damage blood vessels and tissues, prompting the immune system to respond with inflammation to repair the damage. This creates a vicious cycle, where both insulin resistanceand chronic inflammation contribute to long-term issues like weight gain, fatigue, cardiovascular disease, and even type 2 diabetes.
Think of this like a kid (sugar) asking a parent (cells) for something. The kid asks in a normal voice (insulin) and the parent says “no”, the kid screaming at a higher volume (more insulin) still doesn’t make the parent say “yes”. The parent is resistant, and now the parent is annoyed too (inflammation). It also makes the parent more likely to start tuning out the kid, leading to more stress all around.
Insulin resistance happens both because the cells are overloaded with energy and because they become dysfunctional due to chronic stress, inflammation, and excess insulin production. This also has a ripple effect on other glands. Constant blood sugar highs/lows can signal to the pituitary that the body is in a chronic stress state, impacting hormone production. Stress on the thyroid due to insulin resistance or blood sugar fluctuations can contribute to fatigue, weight gain, and mood swings. Frequent blood sugar spikes can cause chronic cortisol release, putting strain on the adrenals and leading to energy crashes, difficulty sleeping, and increased cravings. This is why lifestyle changes like improving diet, managing stress, and increasing physical activity are key to reversing insulin resistance.
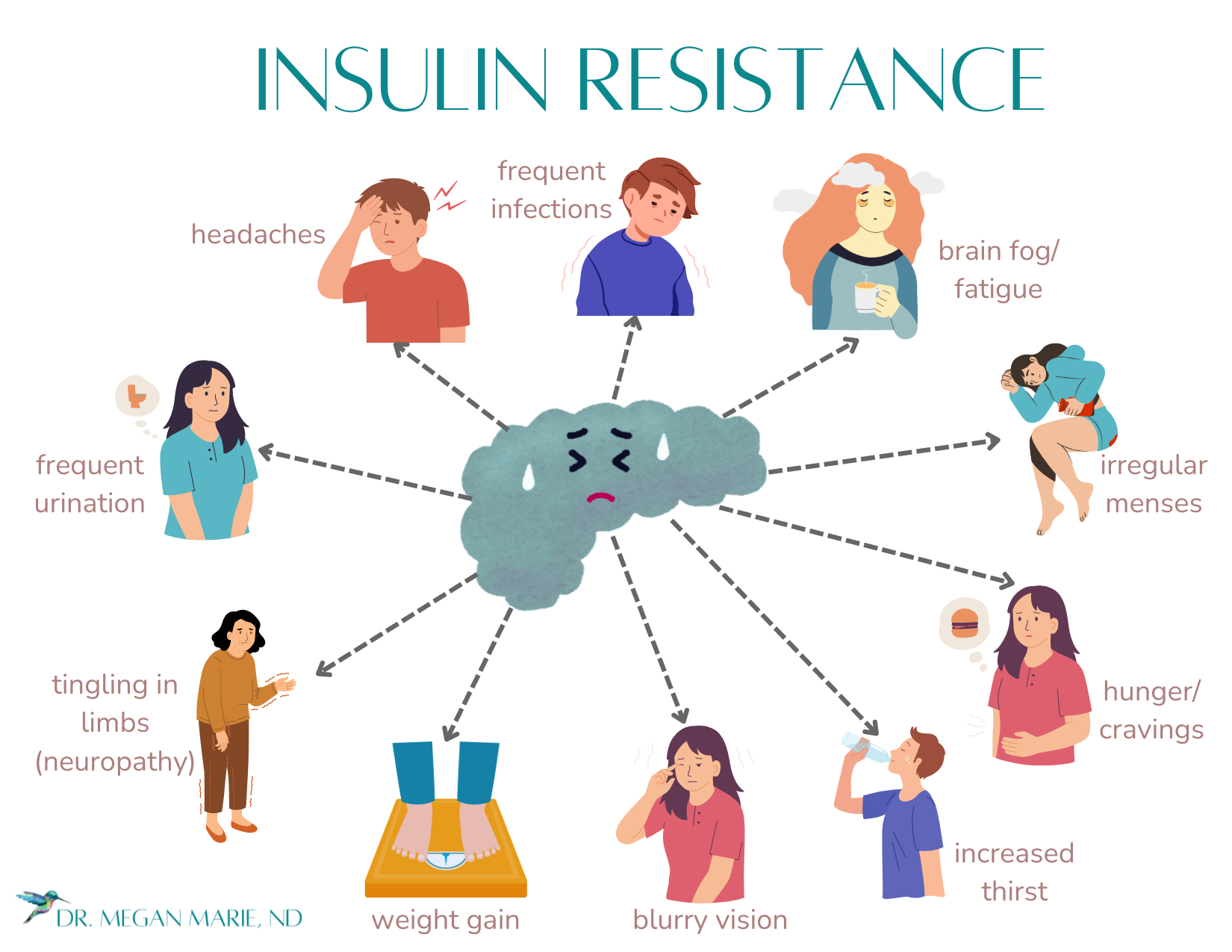
HOW DO YOU KNOW IF YOU HAVE INSULIN RESISTANCE?
Insulin resistance impacts the whole body (because our blood vessels go everywhere), and thus it has non-specific signs when you look at them individually, but collectively…. Signs and symptoms include: fatigue, increased thirst, high blood sugar, sweet cravings, blurred vision, frequent urination, brain fog, frequent infections, tingling (or lack of) sensation in your hands or feet, irregular menses, hunger, high blood pressure, headaches, weight gain.
If you have several signs or symptoms, please reach out to a health provider. And when you do, they’ll likely (should) run some blood tests. These are all conventional labs, meaning you don’t need an expensive specialty lab to get some answers.
FASTING PLASMA GLUCOSE – this one is usually included in a CMP (comprehensive metabolic panel), if you’re fasting. Fasting, meaning no caloric intake for at least 8 hours. Plasma glucose, meaning how much sugar is in the liquid portion of your blood. A conventional doc will tell you this should be less than 100 mg/dL. However, I would say optimally this value should really be between 65-80 mg/dL. Remember, conventional docs wait until things are already boiling over to intervene. That’s what they’re trained to do, save your life. Naturopathic, integrative, alternative, holistic, or “other than conventional” docs tend to turn down the heat when things are just starting to simmer. Hence: optimal vs. conventional lab values. If a FPG is great than 126 mg/dL, two or more times, this is diagnostic of type 2 diabetes.
HEMOGLOBIN A1C (HbA1c) – is a blood test that measures the amount of glucose (sugar) attached to hemoglobin (the protein in red blood cells that caries oxygen). You know how when you get sugar water on your hands, your hands get sticky? Same with your blood. Your HbA1c measures the average amount of sugar in your blood over the past three months. A healthy HbA1c is between 4.8-5.6. If it’s between 5.7-6.4 it’s considered pre-diabetes; at 6.5 or above it's considered type 2 diabetes. Start sitting up and taking notice if your HbA1c is creeping towards 5.4 or 5.5 and you’re having any of the above symptoms.
IMPAIRED GLUCOSE TOLERANCE (IGT) – this test requires that you drink 75mg of oral glucose. For this they compare the pre-test glucose value, with the glucose at typically 30 minutes, one hour, and two hours. It’s the gold-standard for evaluating how the body is responding to blood sugar over time, but it’s pretty uncomfortable. You’re eating a lot of sugar, and then not eating anything for two hours, I can really make you feel awful. Plus, it’s two hours at a lab. I don’t run this one if I don’t have to.
INSULIN – this is often not ordered by conventional practitioners. Insulin resistance can be there years before we start to show overt signs of disease and even long before we have chronically high blood sugar (hyperglycemia). A study involving the Pima, showed these individuals were insulin resistant anywhere between 5-12 years before developing diabetes, and it was highly predictive of their developing diabetes. Insulin should optimally be between 5-10µIU/mL, and not above 30µIU/mL, in the conventional world, it’s even higher. However, “the lower the better” does not apply. Insulin needs to be above 2µIU/mL, otherwise this suggests poor pancreatic production. To review: if it’s too high it suggests your cells are ignoring insulin and it’s staying in your blood (insulin resistant) and if it’s too low, your pancreas has thrown in the towel, and you’re not producing enough (insulin deficient).
EAT (AND MOVE) TO LIVE
There isn’t one right diet for everyone. You’ll find amazing evidence on eating anyway from plant-based to paleo, with pretty strong camps for both. What they both agree on however is to eat real food. And that’s the camp I’m in. Focus on eating vegetables, fruits, fiber, unsaturated fats (avocado, olive oil), nuts and seeds, and whole grains (yes, whole grains, especially women, grains in the evening help us sleep, and lose weight). Avoid saturated fats, trans fats, processed carbs or sugars, natural or artificial flavors (and things you can’t pronounce).
Remember, this is all easier said than done. There is BIG money invested in making you crave the crap (why does it have to taste so good if it’s so bad?).
Be compassionate with yourself. Start by adding in the good, and that’ll naturally start crowding out the bad.
Likewise, even just 30 minutes of brisk walking can help you start moving and get that blood sugar out of your cells (and boost your mood, especially if you can walk in nature).
That was a lot, you’ve learned so much! Thank you for reading and continuing to join me on this “Tour of the Body” series. The more you know about your body, and how it works, the more empowered you can be with how to take care of you!
PITUITARY GLAND: THE REGULATOR
THYROID GLAND: THE METABOLISM MANAGER
ADRENAL GLANDS: THE STRESS RESPONDER
PANCREAS (REVISITED): THE SUGAR REGULATOR
GONADS: THE MIRACLE & STRUCTURAL MAKERS
PINEAL GLAND: THE SLEEPER & HEALER